7 Common Questions About Spinal Cord Stimulation
Frequently Asked Questions about SCS
Spinal Cord Stimulation (SCS) is an exciting treatment option for patients who suffer from chronic back pain. SCS is a minimally invasive surgery that offers an option for patients whose back or neck pain isn’t fully managed from other treatments, such as opioids or other medications. This treatment is an effective alternative to opioid medication and traditional chronic pain therapies.
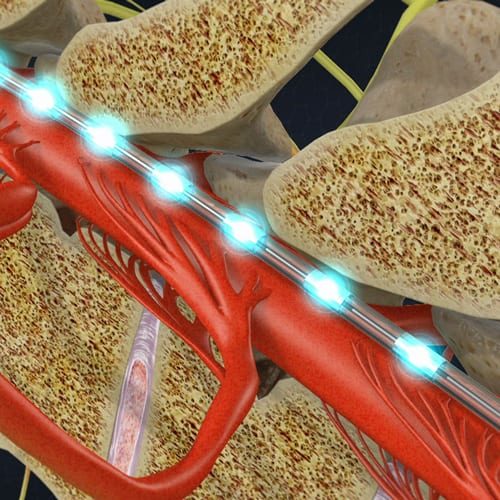
1. What Does Spinal Cord Stimulation Do?

We often describe Spinal Cord Stimulation as being a “pacemaker for pain.” SCS therapy is an implanted device with leads running to the nerves in your spine. These leads deliver electrical impulses to the nerves that essentially disrupt pain signals before they can reach your brain. Spinal cord stimulation devices are approved by the U.S. Food and Drug Administration (FDA) to target and treat chronic pain of the arms, legs and trunk, or pain resulting from failed back surgeries, chronic pain, or other spine injuries.
2. Do Spinal Cord Stimulators Actually Work?
Patients we’ve treated with spinal cord stimulation have reported significant relief over 80% of the time. This treatment is very effective for treating certain types of chronic pain related to nerve and tissue damage, as well as failed back surgery syndrome and pain caused spinal disorders.
While complete pain relief is not guaranteed, a greater than 50% decrease in reported pain is commonly reported. Patients will undergo a trial procedure where a temporary SCS is placed for 5-10 days. The trial helps patients and our doctors learn how to use the system, develop a comfort with how it feels, and gauge what degree of pain relief it provides. The trial provides a prognostic guide for how much pain relief the SCS will provide long term.

3. Does Spinal Cord Stimulation Cause Numbness or Tingling?
Previous generations of spinal cord stimulators interrupted pain signals using a sensation called “paresthesia” which could be described as tingling or prickling. This sensation, while effective, could cause disruptions or discomfort in day-to-day life.
SpineOne uses a newer form of SCS therapy called HF-10, or high-frequency spinal cord stimulation. High frequency stimulation offers pain relief without a tingling sensation. HF10 can be left on 24 hours a day, 7 days a week because it calms the nerves without delivering disruptive or distracting sensations.
4. Will the SCS Implant Be Visible?
It’s a common misconception that the implant will be visible under your skin, or that you’ll be able to feel it. The module is small and implanted in such a way that you’d never notice it. The HF10 implants are small and oval shaped. Your doctor will position it in a comfortable, convenient, and unobtrusive location. The only way someone will know you have it is if you tell them.

5. Can I Get an MRI with a Spinal Cord Stimulator?
Most newer models of spinal cord stimulators are now MRI compatible. Discuss your stimulator with the doctor requesting your MRI, including a detailed description of your devices, including the product number of the Implant, leads, and other implanted components. Prior to your MRI scan, make sure your stimulation is turned off. Your stimulator can resume normal function after your scan.
6. Will a Spinal Cord Stimulation Mean Less Pain Medication?
The results of SCS therapy vary from patient to patient. Using a spinal cord stimulator in no way means you can’t use pain medication if you require it, but it will likely mean you require it less (or not at all!). Some of our patients have reported that they’re no long reliant on pain medication for their day to day lives. For others, success has meant reduction in medication requirements. On average, four out of five of our patients report that HF10 therapy has resulted in significant reduction in their pain medication use.

7. How Do I Choose the Right Doctor for Spinal Cord Stimulation?

Choosing the right doctor for spinal cord stimulation is imperative. You want a doctor who has a proven track record of successful procedures, as well as an established expertise with chronic pain, spinal disorders, and various treatment methods. Doctors who are fellowship-trained in pain management are ideal for this procedure. These doctors are highly skilled in the diagnosis and treatment of pain due to their additional training exclusively within the field of pain management.


